An Early Clinical Case of COVID-19 in New York
An Early Clinical Case of COVID-19 in New York
(1) Peter Capainolo, FLS and (2) Ronald M. Chase, MD
1. Division of Vertebrate Zoology, American Museum of Natural History, CPW@79th Street
New York, NY 10024-5192 pcap@amnh.org
2. 551 Rylane Street, DeLeon Springs, FL 32130 DRPTSD@aol.com
1. Summary
SARS-CoV-2, a novel coronavirus that causes the disease COVID-19 in humans spread rapidly from its origins in Wuhan, China to multiple countries. 517,136,487 cases have been reported as of 8 May 2022 (https://www.worldometers.info/coronavirus/). The first case in the United States reportedly occurred on 20 January 2020 in Washington state in a patient with a history of travel to Wuhan (Holshue et al. 2020). We report an earlier case of COVID-19 in Queens, New York in November 2019.
2. Case Report
On 6 November 2019, a 60-year-old Caucasian male with a five-day history of wet cough, headache, subjective fever, and dyspnea presented to the emergency department of the Mount Sinai Hospital in New York City after visiting an urgent care clinic where his oxygen saturation levels were found to be low (90-93%). The patient, a long-time resident of Queens, New York, reported becoming acutely ill on the evening of 2 November 2019 while attending a conference of approximately one hundred people in upstate New York (Otsego County). Assuming influenza, he self-isolated at the home of a friend in Ulster County, New York, from 3-5 November. His host did not subsequently become ill, and it is not known if any of the conference attendees reported similar symptoms. His partner, a 51-year-old Haitian American female and licensed practical nurse, became ill with similar signs and symptoms shortly after picking him up from Ulster County. She did not seek treatment, and her illness fully resolved within a month. Both the patient and his partner subsequently tested positive for serum IgG antibodies to SARS-CoV-2.
3. Emergency Department Findings and Diagnostic Evaluation
The patient’s medical history includes coronary artery disease (CAD) and a sustained myocardial infarction in 2007. He was treated with angioplasty and staged stent placement, the most recent of 11 total stents was placed in 2017. Management of his CAD and associated hypertension and hyperlipidemia included: aspirin 81mg, losartan 25 mg, isosorbide 60 mg, atorvastatin 80 mg, metoprolol 50 mg and niacin 500 mg. Since 1989 symptoms of depression and anxiety have been controlled by fluoxetine 20 mg. A reducible umbilical hernia was noted. Past surgical history included lithotripsy and cystoscopy for renal calculi.
4. Physical examination, Laboratory Findings and Admission to Hospital     The patient is a 60-year-old white male with a Body Mass Index (BMI) >30, afebrile, and not in acute distress. Symptoms include a five-day history of subjective fever, headache, wet cough, chills, myalgia, sore throat, and dyspnea. Patient denied nausea, vomiting, abdominal pain, or urinary symptoms. On arrival to the emergency department blood pressure was 136/71, pulse 74, respiration 20, and temperature was 97.1℉. Oxygen saturation level was 96% but subsequently fell to 92-93%. Auscultation of chest was positive for scattered rhonchi. Placement on 2L NC effected improvement to 97%. Patient was started on IV ceftriaxone and azithromycin to cover possible bacterial etiology. At this time, the patient was admitted to hospital. Serology over three days was mostly unremarkable but several abnormal values indicating infection and low oxygen levels were noted (Fig.1). Computed Tomography Angiography (CTA) of the lungs was ordered to rule out pulmonary embolism and pneumonia but showed multiple, scattered, indeterminate ground-glass nodular opacities and diffuse bronchial wall thickening (Fig. 2). A nasal swab returned a positive PCR result for Influenza A on Rapid Influenza Diagnostic Test (RIDT).Â
| Serology 11/06/2019 | Value | Serology 11/07/2019 | Value | Serology 11/08/2019 | Value |
| ANION GAP (mEq/L) | 9.7 | TROPONIN-1 (NG/ML) | 0.02 | ANION GAP (mEq/L) | 9.8 |
| BASE EX.VEN (POCT) (%) | 4.0 (H) | PROCALCITONIN (ng/mL) | 0.06 | BASOPHIL # (x10E3/uL) | 0 |
| BASOPHIL # (x10E3/uL) | 0 | BASOPHIL (%) | 0.5 | ||
| BASOPHIL (%) | 0.6 | CALCIUM (mg/dL) | 8.2 (L) | ||
| CALCIUM (mg/dL) | 8.6 | CHLORIDE-BLD (MEQ/L) | 109 (H) | ||
| CHLORIDE-BLD (MEQ/L) | 108 | CO2 TOTAL (MEQ/L) | 23.2 | ||
| CO2 TOTAL (MEQ/L) | 22.3 | CREATININE (mg/dL) | 1.03 | ||
| CREATININE (mg/dL) | 1.19 | EOSINOPHIL # (x10E3/uL) | 0 | ||
| EOSINOPHIL # (x10E3/uL) | 0 | EOSINOPHIL (%) | 0.6 | ||
| EOSINOPHIL (%) | 0.7 | GLUCOSE (mg/dL) | 105 (H) | ||
| GLUCOSE (mg/dL) | 110 (H) | HEMATOCRIT (%) | 45.9 | ||
| HCO3.VEN (POCT) (MEQ/L) | 29 (H) | HEMOGLOBIN (G/DL) | 15.4 | ||
| HEMATOCRIT (%) | 47.3 | LYMPHOCYTE # (x10E3/uL) | 1.1 | ||
| HEMATOCRIT-VEN (POCT) (%) | 47 | LYMPHOCYTE (%) | 27.3 | ||
| HEMOGLOBIN (%) | 15.9 | MEAN CORP.HGB (PG) | 31.2 | ||
| LYMPHOCYTE # (x10E3/uL) | 1.3 | MEAN CORP.HGB CONC. (G/DL) | 33.6 | ||
| LYMPHOCYTE (%) | 26.3 | MEAN CORP.VOLUME (FL) | 93 | ||
| MEAN CORP.HGB (PG) | 30.9 | MEAN PLT VOLUME (FL) | 8.5 | ||
| MEAN CORP.HGB CONC. (G/DL) | 33.6 | MONOCYTE # (x10E3/uL) | 0.8 | ||
| MEAN CORP.VOLUME (FL) | 92.2 | MONOCYTE (%) | 19.7 (H) | ||
| MEAN PLT VOLUME (FL) | 8.4 | NEUTROPHIL # (x10E3/uL) | 2.1 | ||
| MONOCYTE # (x10E3/uL) | 0.8 | NEUTROPHIL (%) | 51.9 | ||
| MONOCYTE (%) | 15.5 (H) | PLATELET (x10E3/uL) | 102 (L) | ||
| NEUTROPHIL # (x10E3/uL) | 2.8 | POTASSIUM (MEQ/L) | 3.7 | ||
| NEUTROPHIL (%) | 56.9 | RBC BLOOD CELL (x10E3/uL) | 4.94 | ||
| O2 SAT.VEN (POCT) (%) | 67 | RBC MORPHOLOGY-1 | Normal | ||
| PCO2.VEN (POCT) (MM HG) | 45 | RED DISTRIB.WIDTH (%) | 13.9 | ||
| PH.VEN (POCT) | 7.42 | SODIUM-BLD (MEQ/L) | 142 | ||
| PLATELET (x10E3/uL) | 109 (L) | UREA NITROGEN (mg/dL) | 13 | ||
| PO2.VEN (POCT) (MM HG) | 34 | WHITE BLOOD CELL (x10E3/uL) | 4.1 (L) | ||
| POTASSIUM (MEQ/L) | 4.2 | ||||
| Serology 11/06/2019 | Value | Serology 11/07/2019 | Value | Serology 11/08/2019 | Value |
| RBC BLOOD CELL (x10E6/uL) | 5.13 | ||||
| RBC MORPHOLOGY-1 | Slight Ovalocytes | ||||
| RBC MORPHOLOGY-1 | Slight Burr Cells | ||||
| RED DISTRIB WIDTH (%) | 13.9 | ||||
| SODIUM-BLD (MEQ/L) | 140 | ||||
| TOT CO2. VEN (POCT) (MEQ/L) | 31 | ||||
| UREA NITROGEN (mg/dL) | 20 | ||||
| WB CA++. VEN (POCT) (MMOL/L) | 1.05 (L) | ||||
| WB GLUCOSE-VEN (POCT) (mg/dL) | 119 | ||||
| WB K VEN (POCT) (MEQ/L) | 52 (H) | ||||
| WB LACTATE-VEN (POCT) (MMOL/L) | 1.6 | ||||
| WB NA VEN (POCT) (MEQ/L) | 136 | ||||
| WHITE BLOOD CELL (x10E3/uL) | 4.9 |
Figure 1. Patient’s serology results over three days indicating normal and flagged values.
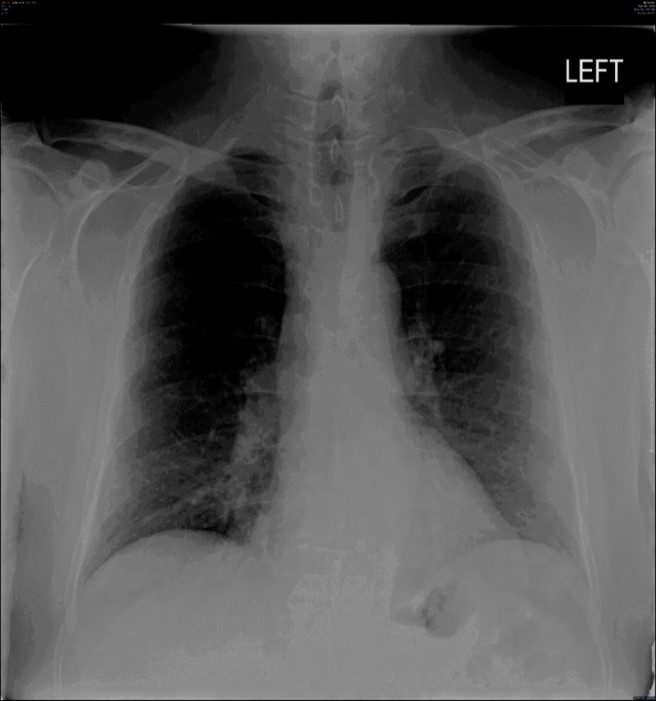
Figure 2. Computed Tomography Angiography (CTA) of the lungs (with contrast) of our patient showing multiple, scattered, indeterminate ground-glass nodular opacities and diffuse bronchial wall thickening.
6. Diagnosis and treatment
Based on clinical signs and symptoms, a positive Influenza A PCR nasal swab test, and non-specific inflammatory findings on lung images, a diagnosis of acute hypoxic respiratory failure secondary to flu was made. IV antibiotics were discontinued, and the patient was prescribed the antiviral Tamiflu (Oseltamivir) 75 mg b.i.d. to be continued for 4 days after discharge from hospital. An inhaled steroid and supplemental oxygen improved the patient’s symptoms while hospitalized and Flovent was prescribed to manage lingering respiratory symptoms after discharge on 8 November 2019. A follow-up appointment with his primary care physician was scheduled for 14 November 2019.
7. Follow-up
The patient was seen by his primary care physician 6 days later. No issues of concern were noted. He was afebrile, without cough and lung sounds were normal. On 8 May 2020, well into the COVID-19 pandemic, the patient self-referred to the originally visited urgent care clinic regarding the similarity in clinical features to his condition in November 2019. A SARS CoV-2 serum antibody test was positive (7.1) for IgG antibodies to SARS CoV-2 (+ = >1.4). On 19 August 2020, prior to a previously scheduled biopsy for a laryngeal granuloma, protocol required him to undergo the nasal swab PCR test for SARS CoV-2 antigens. The result was negative. Finding the clinical picture and positive IgG antibody to novel coronavirus interesting, the patient’s primary medical provider ordered another serum antibody assay on 14 October 2020. This returned a moderate positive titer of 320. A positive result on the SARS-CoV-2 Antibody Spike, Semi-quantitative test (78.20 U/mL) taken on 1 August 2021 indicated long-lasting immunity. On 17 February 2022, the patient was tested for memory T-cell adaptive immunity to SARS CoV-2 which returned a positive result suggesting long-lasting protection from reinfection (Wang et al. 2021). Considering these findings, in part, the patient applied for, and was granted, a medical exemption from COVID-19 vaccination required by his employers. His accommodation requires weekly testing (by nasal swab) for SARS CoV-2 antigen. As of this writing he has been tested > 25 times all with negative results and has been asymptomatic since his hospital admission in early November 2019.
8. Discussion
The presentation, clinical findings and course of disease suggest an early case of COVID-19 in New York that predates the first reported case from Washington state by over two months. In addition to constitutional symptoms now known to be common in the disease, the patient had lung manifestations that, while not pathognomonic for COVID-19 sensu stricto, are currently well known in the literature on COVID-19 (An et al. 2020, Han et al. 2020, Kong et al. 2020, Wang et al. 2020, Xie et al. 2020). That the patient subsequently tested positive for serum antibodies and an adaptive T-cell immune response to SARS Co-V-2 confirm infection with SARS Co-V-2. Demographic and temporal factors should be considered in this case as well. The patient lives in the New York borough of Queens, parts of which have high populations of Chinese immigrants, some of whom may have attended the Olympic games in Wuhan in October of 2019 (http://www.xinhuanet.com/english/2019-10/18/c_138483351.htm) became infected, and returned home with the first cases on the east coast earlier than November 2019.
The most confounding factor in this case is the positive RIDT taken in the emergency department which elucidated a diagnosis and change in treatment course. Explanations include a false positive RIDT (Chartrand et al. 2012) and the phenomenon of co-infection with coronavirus disease and influenza (Hashemi et al. 2020 & Khodamoradi et al. 2019). Another possibility is that the original disease was influenza, and the patient later sustained an asymptomatic case of COVID-19 which produced the immune response. The robust IgG response suggest otherwise as do the patients subjective sense that past bouts with influenza felt different than this disease which lacked high fever, intestinal or gastric distress and other common features of influenza virus infection.
9. OVERVIEW
In a pandemic era, this exemplar’s presentation, constellation of symptoms and laboratory findings, would urge a viral etiologic agent. Epidemiologic factors would command correlation to be causation. Despite the paucity of constitutional symptoms at the outset, laboratory and positive imaging findings would confirm the presence of a viral illness i.e., Coronavirus.
    The longitudinal study of this case does not provide for the earlier history of immunological integrity to determine a de novo viral entity, compromised immune state, or normal integrity of the patient during a pandemic. This case has evolved over the past year with weekly follow up testing, per mandate, for the presence of Coronavirus or COVID-19 which never tested positive. It is suggested that immune test baseline parameters be established before administration of preventive measures, antiviral treatment, or vaccination be undertaken.
References
An, P., Song, P., Lian, K. and Wang, Y., 2020. CT manifestations of novel coronavirus pneumonia: a case report. Balkan medical journal, 37(3), p.163.
Chartrand, C., Leeflang, M.M., Minion, J., Brewer, T. and Pai, M., 2012. Accuracy of rapid influenza diagnostic tests: a meta-analysis. Annals of internal medicine, 156(7), pp.500-511.
Hashemi, S.A., Safamanesh, S., Ghafouri, M., Taghavi, M.R., Mohajer Zadeh Heydari, M.S., Namdar Ahmadabad, H., Ghasemzadehâ€Moghaddam, H. and Azimian, A., 2020. Coâ€infection with COVIDâ€19 and influenza A virus in two patients with acute respiratory syndrome, Bojnurd, Iran. Journal of medical virology, 92(11), pp.2319-2321.
Holshue, M.L., DeBolt, C., Lindquist, S., Lofy, K.H., Wiesman, J., Bruce, H., Spitters, C., Ericson, K., Wilkerson, S., Tural, A. and Diaz, G., 2020. First case of 2019 novel coronavirus in the United States. New England Journal of Medicine.
http://www.xinhuanet.com/english/2019-10/18/c_138483351.htm
https://www.worldometers.info/coronavirus/
Han, R., Huang, L., Jiang, H., Dong, J., Peng, H. and Zhang, D., 2020. Early clinical and CT manifestations of coronavirus disease 2019 (COVID-19) pneumonia. American Journal of Roentgenology, 215(2), pp.338-343.
Khodamoradi, Z., Moghadami, M. and Lotfi, M., 2020. Co-infection of coronavirus disease 2019 and influenza: a report from Iran.
Kong, W. and Agarwal, P.P., 2020. Chest imaging appearance of COVID-19 infection. Radiology: Cardiothoracic Imaging, 2(1), p.e200028.
Wang, Y., Dong, C., Hu, Y., Li, C., Ren, Q., Zhang, X., Shi, H. and Zhou, M., 2020. Temporal changes of CT findings in 90 patients with COVID-19 pneumonia: a longitudinal study. Radiology, 296(2), pp. E55-E64.
Xie, X., Zhong, Z., Zhao, W., Zheng, C., Wang, F. and Liu, J., 2020. Chest CT for typical coronavirus disease 2019 (COVID-19) pneumonia: relationship to negative RT-PCR testing. Radiology, 296(2), pp. E41-E45.
Wang, Z., Yang, X., Zhong, J. et al. Exposure to SARS-CoV-2 generates T-cell memory in the absence of a detectable viral infection. Nat Communications 12, 1724 (2021). https://doi.org/10.1038/s41467-021-22036-z